Beyond the Needle: Understanding and Overcoming Vaccine Hesitancy
Commentary - (2024) Volume 13, Issue 2
Description
Issue of vaccine hesitancy, which is influenced by psychological, social, and cultural factors. It examines how historical mistrust, fear of side effects, and misinformation contribute to reluctance in accepting vaccines. The work highlights the importance of effective communication strategies, including personalized messaging and community engagement, to address concerns and build trust. It also discusses policy approaches and real-world case studies where vaccine hesitancy has been successfully mitigated, offering insights for public health initiatives aimed at increasing vaccine acceptance. Vaccine hesitancy refers to the delay in acceptance or refusal of vaccines despite the availability of vaccination services. This phenomenon poses a significant challenge to public health, as it can lead to outbreaks of preventable diseases and hinder efforts to achieve herd immunity. Vaccine hesitancy is influenced by a complex mix of factors, including misinformation, distrust in government or medical authorities, concerns about vaccine safety, religious or cultural beliefs, and the perceived low risk of diseases due to their rarity in vaccinated populations. The spread of misinformation, particularly through social media, has amplified fears and misconceptions, making it harder to convince certain groups of the benefits of vaccination.Vaccines have long been heralded as one of the most effective tools in preventing infectious diseases and promoting public health. However, in recent years, vaccine hesitancy has emerged as a significant global challenge, undermining vaccination efforts and posing risks to individual and community immunity. Vaccine hesitancy refers to a delay in acceptance or refusal of vaccines despite the availability of vaccination services. This hesitancy is influenced by a complex interplay of factors, including concerns about vaccine safety, misinformation spread through social media and other channels, mistrust in healthcare providers or government authorities, and religious or philosophical beliefs. The consequences of vaccine hesitancy are far-reaching. Outbreaks of vaccine-preventable diseases, such as measles, mumps, and whooping cough, have reemerged in communities with low vaccination rates, leading to increased morbidity and mortality among vulnerable populations, including children, the elderly, and individuals with compromised immune systems. Addressing vaccine hesitancy requires a multifaceted approach that includes enhancing public understanding of vaccines and their safety, improving communication between healthcare providers and patients, and countering misinformation through evidence-based education campaigns. Building trust in vaccines and the healthcare system is essential to fostering confidence in vaccination among hesitant individuals and communities. Healthcare providers play a crucial role in addressing vaccine hesitancy by engaging in open and respectful conversations with patients, addressing concerns about vaccine safety and efficacy, and emphasizing the benefits of vaccination for individual and community health. By addressing concerns and providing accurate information, healthcare providers can help empower individuals to make informed decisions about vaccination. On a global scale, collaboration among governments, healthcare organizations, and community leaders is essential. Efforts to strengthen immunization programs, improve access to vaccines, and monitor vaccine safety are critical components of combating vaccine hesitancy and promoting widespread vaccine acceptance. While addressing vaccine hesitancy is a complex and ongoing challenge, the benefits of vaccination in preventing infectious diseases and protecting public health cannot be overstated. By working together to address concerns, build trust, and promote evidence-based vaccination practices, we can overcome vaccine hesitancy and ensure a healthier future for generations to come.
Acknowledgement
The authors are very thankful and honoured to publish this article in the respective Journal and are also very great full to the reviewers for their positive response to this article publication.
Conflict Of Interest
We have no conflict of interests to disclose and the manuscript has been read and approved by all named authors.
Author Info
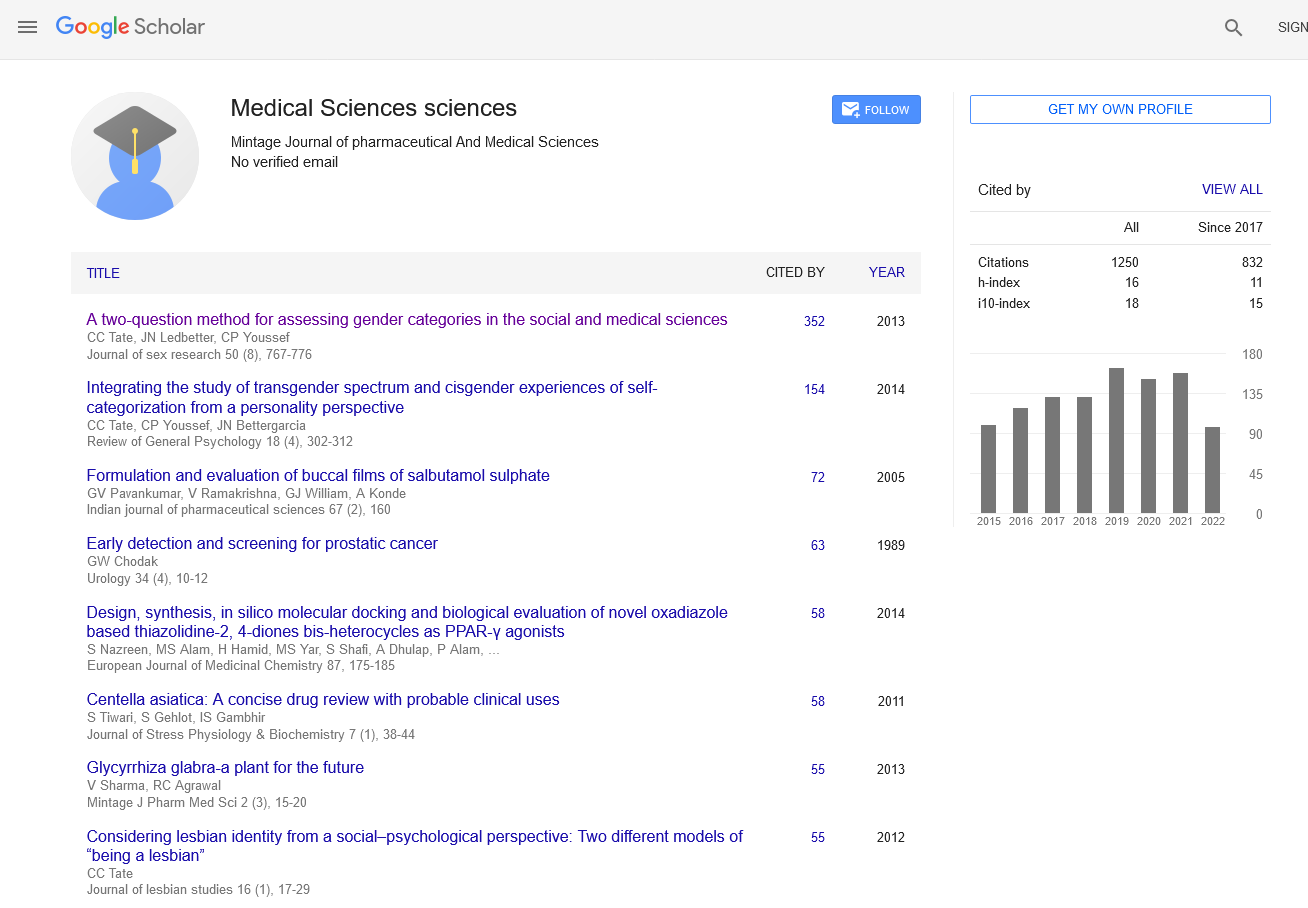
Rony Dev*Received: 29-May-2024, Manuscript No. mjpms-24-141845; , Pre QC No. mjpms-24-141845 (PQ); Editor assigned: 31-May-2024, Pre QC No. mjpms-24-141845 (PQ); Reviewed: 14-Jun-2024, QC No. mjpms-24-141845; Revised: 19-Jun-2024, Manuscript No. mjpms-24-141845 (R); Published: 26-Jun-2024, DOI: 10.4303/2320-3315/236014
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

ISSN: 2320-3315
ICV :81.58