Empowering Psychologists with Prescriptive Authority: A Progressive Step for Mental Health Care in India
Commentary - (2024) Volume 13, Issue 2
Description
In the rapidly evolving landscape of mental health care, there is an urgent need to re-evaluate and expand the roles and responsibilities of mental health professionals. In India, psychologists play a crucial role in addressing the burgeoning mental health crisis. However, their capacity to deliver comprehensive care is significantly limited by their inability to prescribe medication. Advancing psychopharmacological training and granting prescriptive authority to qualified psychologists could transform mental health care in India, leading to more integrated, accessible, and effective treatment options for patients. The mental health crisis in India is staggering. According to the National Mental Health Survey of India 2015-16, nearly 15% of Indian adults require active intervention for one or more mental health issues. Despite this high prevalence, there is a severe shortage of mental health professionals, particularly psychiatrists, who are authorized to prescribe psychotropic medications. This shortage exacerbates the treatment gap, leaving millions without the comprehensive care they need. Empowering psychologists with prescriptive authority could alleviate some of this burden, providing timely and holistic care to patients. To achieve this, it is essential first to enhance the psychopharmacological training of psychologists. Currently, the educational curriculum for psychologists in India predominantly focuses on psychological theories, therapeutic techniques, and research methodologies. While these are vital components of their training, there is a noticeable gap in their education regarding psychopharmacology and the biological underpinnings of mental disorders. Introducing specialized courses and practical training in psychopharmacology within the psychology curriculum would equip psychologists with the knowledge and skills required to prescribe medications safely and effectively. Moreover, the implementation of rigorous certification and licensure processes is crucial to ensure that only those psychologists who have demonstrated a high level of competency in psychopharmacology are granted prescriptive authority. This would involve a combination of theoretical examinations, practical assessments, and supervised clinical experience. Establishing such stringent criteria would help maintain high standards of care and protect patient safety. In addition to enhancing training and certification, fostering collaboration between psychologists and psychiatrists is paramount. A collaborative model of care, where psychologists with prescriptive authority work alongside psychiatrists, can ensure a more comprehensive and coordinated approach to treatment. This collaboration can also facilitate continuous learning and professional development for psychologists, as they benefit from the expertise and experience of their psychiatrist colleagues. Granting prescriptive authority to psychologists is not without its challenges and concerns. Critics argue that psychologists may lack the medical training required to prescribe medications safely. However, international examples demonstrate that with proper training and certification, psychologists can prescribe safely and effectively. In the United States, for example, several states have granted prescriptive authority to appropriately trained psychologists, resulting in positive outcomes and increased access to mental health care. Addressing the legal and regulatory aspects of granting prescriptive authority to psychologists in India is also essential. Clear guidelines and regulations must be established to outline the scope of practice, supervision requirements, and continuing education mandates. The involvement of professional bodies, such as the Rehabilitation Council of India (RCI) and the Indian Psychiatric Society (IPS), in developing these regulations is crucial to ensure that the interests of all stakeholders are considered, and patient safety is prioritized. Furthermore, public awareness and acceptance of psychologists as prescribers are vital for the success of this initiative. Educational campaigns highlighting the rigorous training and certification processes that psychologists undergo can help build public trust and confidence in their prescriptive authority. Additionally, involving patients in the decision-making process and respecting their preferences for treatment can foster a more patient-centered approach to care. In conclusion, advancing psychopharmacological training and granting prescriptive authority to psychologists in India is a pragmatic and necessary step towards addressing the mental health crisis. By enhancing the training of psychologists, implementing rigorous certification processes, fostering collaboration with psychiatrists, and establishing clear regulatory guidelines, India can create a more integrated and effective mental health care system. This initiative not only has the potential to alleviate the burden on psychiatrists but also to improve access to comprehensive care for millions of individuals suffering from mental health disorders. The time to act is now, and the benefits of such an action are profound and far-reaching.
Acknowledgement
The authors are very thankful and honoured to publish this article in the respective Journal and are also very great full to the reviewers for their positive response to this article publication.
Conflict Of Interest
We have no conflict of interests to disclose and the manuscript has been read and approved by all named authors.
Author Info
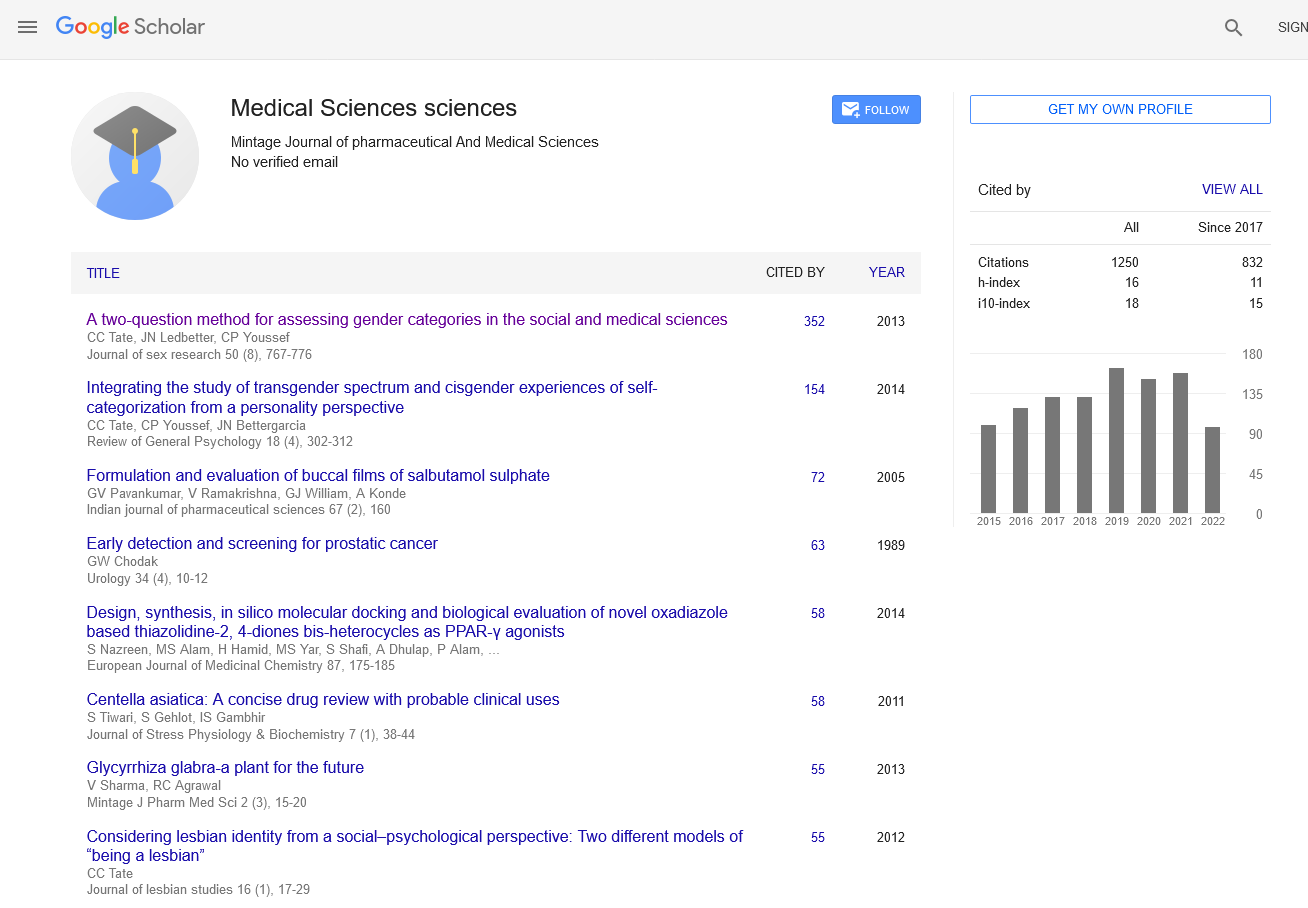
Sofia Silva*Received: 29-May-2024, Manuscript No. mjpms-24-144254; , Pre QC No. mjpms-24-144254 (PQ); Editor assigned: 31-May-2024, Pre QC No. mjpms-24-144254 (PQ); Reviewed: 14-Jun-2024, QC No. mjpms-24-144254; Revised: 19-Jun-2024, Manuscript No. mjpms-24-144254 (R); Published: 26-Jun-2024, DOI: 10.4303/2320-3315/236020
Copyright: © 2024 This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

ISSN: 2320-3315
ICV :81.58