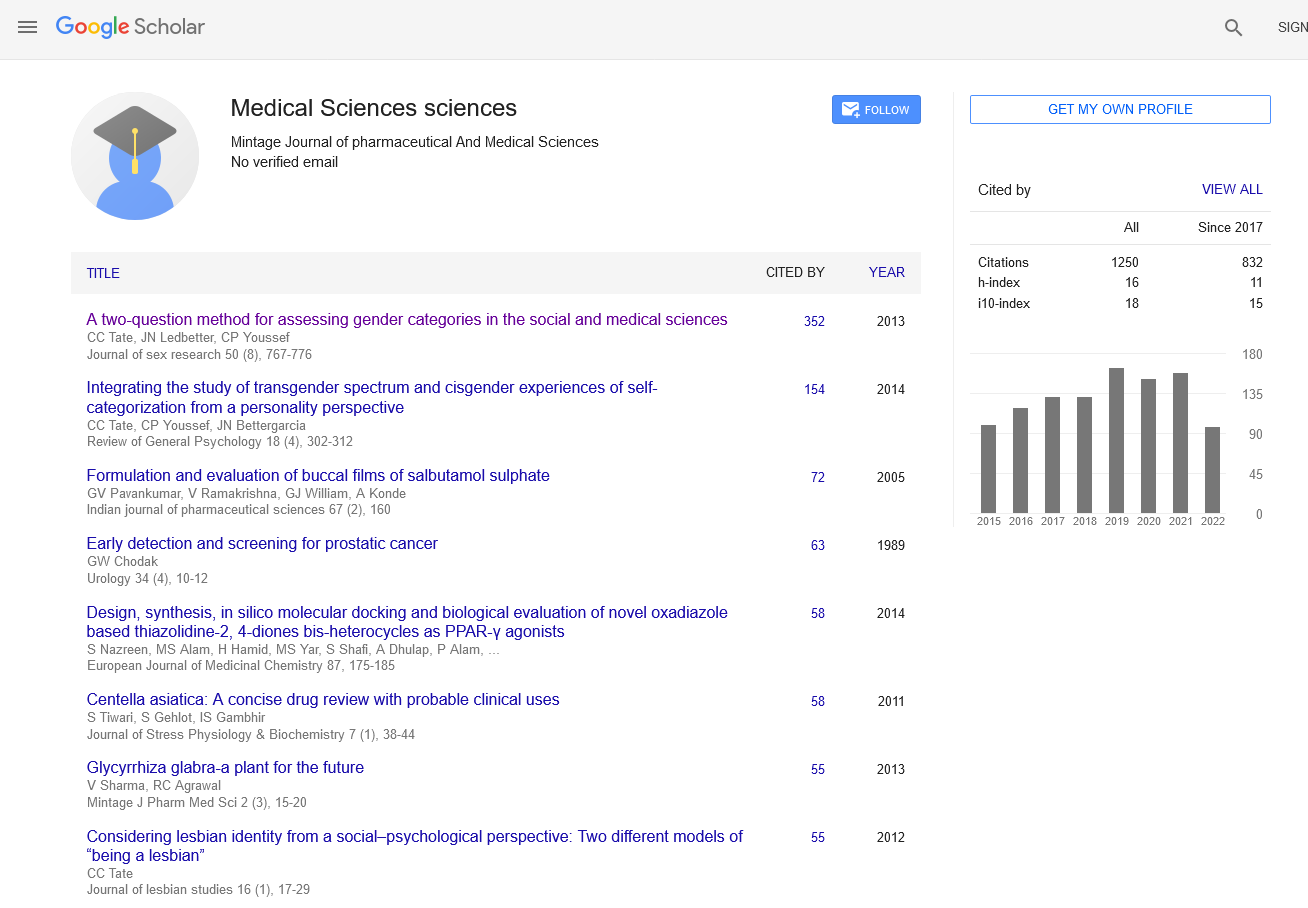
Pharmacogenomics: Understanding Genetic Influences on Drug Response
Opinion - (2024) Volume 13, Issue 2
Introduction
Pharmacogenomics represents a transformative approach in medicine that investigates how an individual’s genetic makeup influences their response to drugs. Unlike traditional medicine, which often adopts a one-size-fits-all approach to drug prescription, pharmacogenomics aims to tailor treatments based on genetic variations among patients. This personalized medicine approach holds promise for optimizing therapeutic outcomes, minimizing adverse drug reactions, and advancing precision healthcare.
Description
At its core, pharmacogenomics explores how genetic variations affect drug metabolism, efficacy, and safety. Genetic differences can significantly influence how drugs are absorbed, distributed, metabolized, and excreted by the body—collectively known as ADME processes. Variants in genes encoding drug-metabolizing enzymes, transporters, and drug targets can alter the pharmacokinetics and pharmacodynamics of medications, leading to variability in treatment responses among individuals. One of the key applications of pharmacogenomics lies in predicting and preventing adverse drug reactions (ADRs). Certain genetic polymorphisms may predispose individuals to metabolize drugs differently, potentially resulting in severe side effects or therapeutic failure. By identifying these genetic markers through pharmacogenetic testing, healthcare providers can preemptively adjust drug dosages or select alternative therapies that are better tolerated and more effective for specific patient profiles. Moreover, pharmacogenomics enhances drug development and clinical trials by enabling researchers to stratify patient populations based on genetic characteristics. This targeted approach not only improves the efficiency of clinical studies but also enhances the likelihood of identifying subgroups that may benefit most from novel treatments. This personalized approach to drug development holds promise for accelerating the translation of genomic discoveries into clinical practice. In oncology, pharmacogenomics plays a pivotal role in guiding the selection of cancer therapies. Genetic testing can identify mutations or biomarkers associated with drug sensitivity or resistance, allowing oncologists to tailor treatment regimens that maximize therapeutic efficacy while minimizing toxicities. This precision oncology approach has revolutionized cancer care by offering patients personalized treatment options based on their unique genetic profiles. Beyond oncology, pharmacogenomics is also shaping the management of cardiovascular diseases, psychiatric disorders, and infectious diseases. Genetic testing can inform medication selection and dosing strategies to optimize treatment outcomes and patient safety across diverse therapeutic areas. As genomic technologies continue to evolve, the integration of pharmacogenomics into routine clinical practice holds promise for improving healthcare outcomes and reducing healthcare costs associated with adverse drug events. Ethical considerations and challenges accompany the implementation of pharmacogenomics in healthcare. Issues such as patient consent, data privacy, equity in access to genetic testing, and the interpretation of complex genetic information require careful consideration and regulatory oversight. Healthcare providers and policymakers must navigate these ethical dilemmas to ensure that pharmacogenomic technologies are deployed responsibly and equitably to benefit patients and populations worldwide.
Conclusion
In conclusion, pharmacogenomics represents a paradigm shift towards personalized medicine, leveraging genetic insights to optimize drug therapy and enhance patient outcomes. By unraveling the genetic underpinnings of drug response variability, pharmacogenomics empowers healthcare providers to deliver tailored treatments that are safer, more effective, and better suited to individual patient needs. As research advances and genomic technologies become more accessible, the widespread adoption of pharmacogenomics promises to usher in a new era of precision healthcare.
Author Info
Enrique Rodraguez*Received: 29-May-2024, Manuscript No. mjpms-24-141867; , Pre QC No. mjpms-24-141867 (PQ); Editor assigned: 31-May-2024, Pre QC No. mjpms-24-141867 (PQ); Reviewed: 14-Jun-2024, QC No. mjpms-24-141867; Revised: 19-Jun-2024, Manuscript No. mjpms-24-141867 (R); Published: 26-Jun-2024, DOI: 10.4303/2320-3315/236015
Copyright: © 2024This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

ISSN: 2320-3315
ICV :81.58