The Rise of Superbugs: Confronting Antibiotic Resistance Worldwide
Short Communication - (2024) Volume 13, Issue 2
Introduction
Antibiotics have long been regarded as one of the greatest achievements in medical science, revolutionizing the treatment of bacterial infections and saving countless lives. However, this once-heralded arsenal against bacterial diseases is now facing a formidable adversary: Antibiotic resistance.
Description
Antibiotic resistance, often referred to as the rise of “superbugs,” is one of the most significant public health challenges of our time. Superbugs are bacteria that have evolved to resist the effects of antibiotics, rendering standard treatments ineffective and leading to more severe infections, longer hospital stays, and increased mortality. The overuse and misuse of antibiotics in human medicine, agriculture, and animal husbandry have accelerated this phenomenon. When antibiotics are used excessively or inappropriately, bacteria adapt quickly, developing mechanisms to survive these drugs. The problem is further compounded by the slow development of new antibiotics, leaving fewer treatment options available. The global impact of antibiotic resistance is alarming, with an estimated 700,000 deaths annually attributed to drug-resistant infections. If current trends continue, this number could rise dramatically, leading to a potential crisis where common infections and minor injuries could become life-threatening.Antibiotic resistance occurs when bacteria evolve in ways that render antibiotics ineffective against them. This natural phenomenon has been exacerbated by the overuse and misuse of antibiotics in human medicine, agriculture, and animal husbandry. The misuse includes unnecessary prescriptions, improper dosing, and failure to complete prescribed courses, all of which contribute to the selection of resistant bacterial strains. The implications of antibiotic resistance are profound and global. Diseases that were once easily treatable with antibiotics, such as pneumonia, tuberculosis, and gonorrhea, are becoming increasingly difficult and sometimes impossible to cure. This shift not only threatens individual health but also poses a significant economic burden on healthcare systems worldwide. The rise of superbugs, or bacteria resistant to multiple antibiotics, further complicates treatment options. Superbugs like Methicillin-resistant Staphylococcus aureus (MRSA) and Carbapenemresistant Enterobacteriaceae (CRE) have emerged as major public health threats, causing severe infections that are challenging to treat and often result in prolonged hospital stays, higher medical costs, and increased mortality rates. Addressing antibiotic resistance requires a multifaceted approach. Enhanced surveillance to monitor resistance patterns, promoting the judicious use of antibiotics through education and guidelines, and developing new antibiotics and alternative treatments are critical strategies. Additionally, improving sanitation, hygiene practices, and infection prevention measures can help reduce the spread of resistant bacteria in healthcare settings and communities. On a global scale, collaboration is essential. International efforts to coordinate policies, share data, and strengthen healthcare infrastructure are necessary to combat antibiotic resistance effectively. Organizations like the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC) play crucial roles in coordinating these efforts and raising awareness about the threat posed by antibiotic-resistant bacteria. Individuals also have a role to play in combating antibiotic resistance. Patients should follow healthcare providers’ advice regarding antibiotic use, including completing prescribed courses and avoiding antibiotics for viral infections like colds and flu. Healthcare providers, in turn, must adhere to prescribing guidelines and adopt antibiotic stewardship practices to optimize antibiotic use and minimize resistance development [1-4].
Conclusion
In conclusion, while antibiotic resistance poses a significant global challenge, it is not insurmountable. By taking decisive action at local, national, and international levels, we can preserve the effectiveness of antibiotics for future generations. The fight against antibiotic resistance requires collective commitment, innovation, and sustained investment in research and public health infrastructure to safeguard antibiotics as a cornerstone of modern medicine.
Acknowledgement
The authors are very thankful and honoured to publish this article in the respective Journal and are also very great full to the reviewers for their positive response to this article publication.
Conflict Of Interest
We have no conflict of interests to disclose and the manuscript has been read and approved by all named authors.
References
- Rathcke B, Lacey EP. Phenological patterns of terrestrial plants. Annu Rev Ecol Syst 1985; 6:16-17.
- Moore LM, Lauenroth WK. Differential effects of temperature and precipitation on early vs. late-flowering species. Ecosphere 2017; 8:e01819.
- Mulik NG, Bhosale LJ. Flowering phenology of the mangroves from the West Cost of Maharashtra. J Bombay Nat Hist Soc 1989; 3:355-339.
- Bareke T. Biology of seed development and germination physiology. Adv Plants Agric Res 2018; 8: 336-346.
Author Info
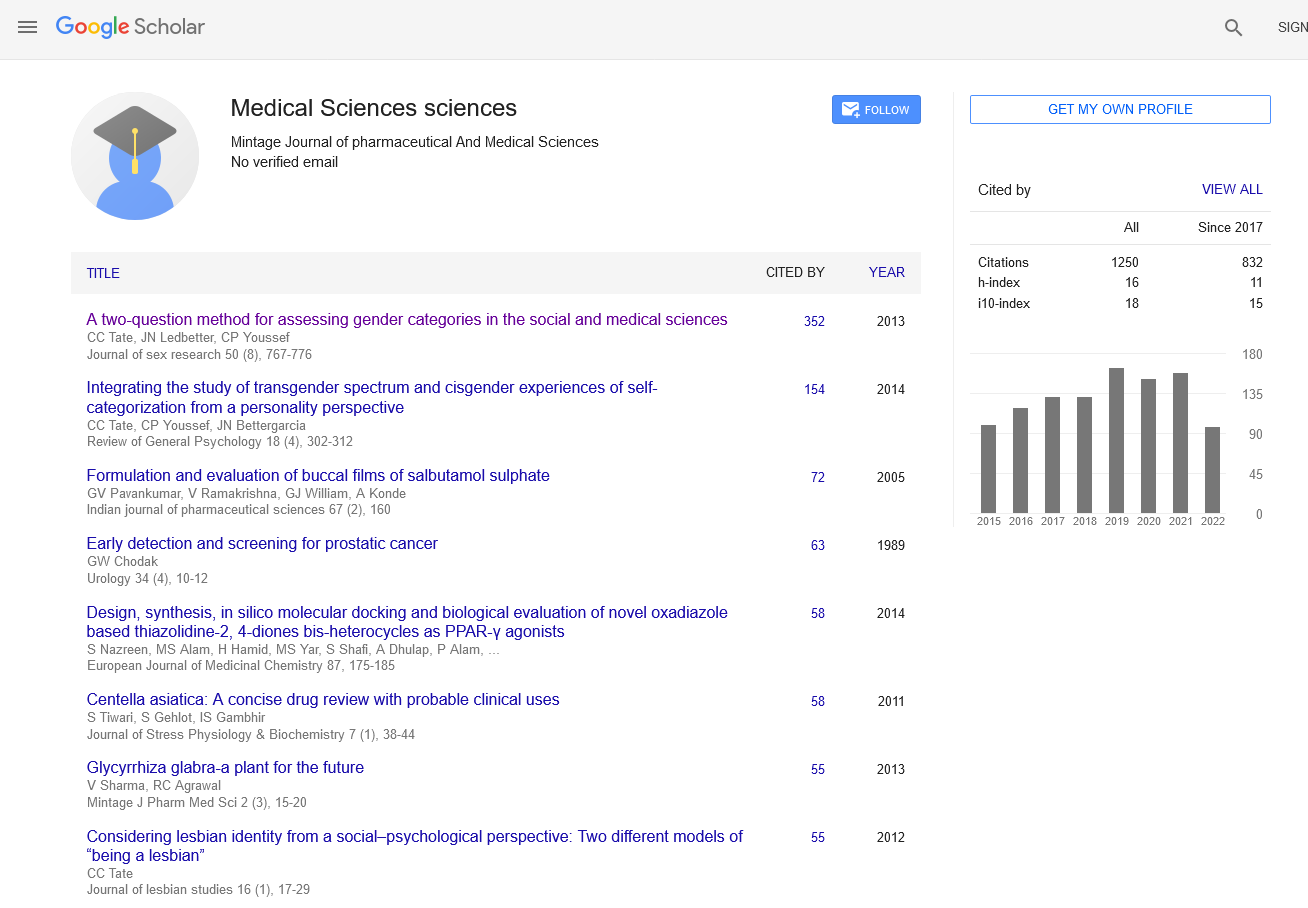
Minglin Zhu*Received: 29-May-2024, Manuscript No. mjpms-24-141840; , Pre QC No. mjpms-24-141840 (PQ); Editor assigned: 31-May-2024, Pre QC No. mjpms-24-141840 (PQ); Reviewed: 14-Jun-2024, QC No. mjpms-24-141840; Revised: 19-Jun-2024, Manuscript No. mjpms-24-141840 (R)); Published: 26-Jun-2024, DOI: 10.4303/2320-3315/236016
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

ISSN: 2320-3315
ICV :81.58